Project Description
Disturbance of consciousness of unknown cause
History:
A 1 year and 4 months old girl was referred by a peripheral hospital due to impaired consciousness of unknown cause. The mother reported, that the child could not be properly roused after having taken a nap at the daycare. The child’s behavior in the morning had been normal.
There was no history of a trauma or infection. The daycare stated, that the child had no access to any drugs or other substances.
In her past medical history there were no major illnesses and her immunizations were up to date.
The mother reported, that the child only called “Mom” once, but was otherwise not communicating with her. To her, the girl seemed to behave very differently than usual.
Clinical findings:
On examination the patient was agitated and only consolable for short periods of time.
Respiration and circulation were stable, except for a slight tachycardia of 113-149 bpm and an arterial hypertension of BD 139/79 mmHg.
The patient did not open her eyes, did not obey commands or react adequately to voice or touch of her mother, but was localizing to pain. There were no lateralization signs, reflexes and muscle tone were normal, but she showed some neck stiffness.
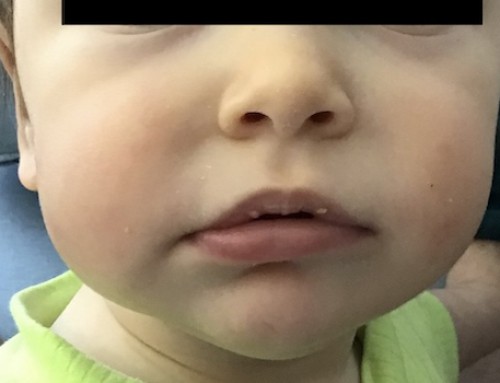
There were no haematoma or other clinical signs for a trauma. There was mild redness of the right upper eyelid. ENT examination was normal.